|
Iritis
Do you have a red eye? Is that red eye sensitive to light? Do you feel a deep, boring pressure type pain in that eye? Has your vision decreased in that eye? You may be suffering from Iritis. What is Iritis?
It is an inflammation of the iris, the colored part of the eye surrounding the pupil. 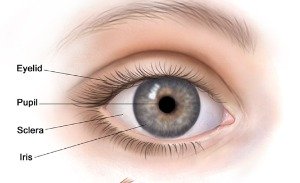
It is a common form of Anterior Uveitis. Iritis can be caused by or associated with the following conditions, such as Blunt Trauma which can result in traumatic inflammation of the iris. Non-traumatic causes can be inflammatory or autoimmune conditions such as: Infectious conditions such as: What are the signs and symptom?

If your Iritis becomes chronic and is left untreated, it can result in Glaucoma and/or Cataracts, which can lead to significant decreased vision. To make sure this eye condition is not missed, you should go to an eye doctor if you have these symptoms. In general, emergency doctor physicians do not have the equipment to properly diagnose Iritis. How is It managed and treated?
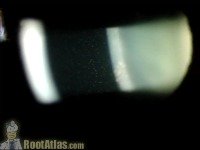
It is best diagnosed by an eye doctor (optometrist or ophthalmologist). Your eye doctor will check your vision, pupillary reactions, and perform a slit lamp examination. A slit lamp is a piece of equipment which serves like a microscope for the eye doctor to view the small structures of your eyeballs. The main clinical finding your eye doctor is looking for is cells floating in the anterior chamber of one or both of your eyes. Cells in the anterior chamber of an eye have been photographed below. They are the white dots in the black-gray area in the center of the picture.
Your eye pressure will be measured. Typically, the eye pressure is low. However, extensive inflammation of the iris and adjacent tissue may actually increase the eye pressure. Your eye pressure can also be elevated from steroid eye drop treatment or insufficient Glaucoma treatment. If you do develop high eye pressure, your eye doctor will prescribe a Glaucoma medication to be added to your treatment regimen. Your affected eye will also be checked for endophthalmitis, which is an active infection inside the eye, and therefore vision-threatening. A classic finding is a pool of white blood cells found at the bottom of the anterior chamber as shown below:
For example, if bacterial, the infection will be treated with antibiotics. As mentioned above, Iritis may be associated with a number of conditions in the body that are inflammatory or infectious in nature. If you have experienced Iritis more than once, or the inflammation is greater severity than average, or both eyes have been affected at the same time, your eye doctor will be more suspicious of a body cause. In order to determine an underlying body disease, laboratory tests and/or referral to Internal Medicine specialist will be done. It will be treated aggressively once the possibility of infection is ruled out with steroid eye drops prescribed every hour or every two hours until a significant impact is made on the inflammation. Remember steroids must be tapered gradually or you risk the inflammation coming back worse than previously. Steroids will be tapered slowly beyond the point that your eye(s) look white and quiet to make sure that the inflammation is adequately eliminated. Your eye doctor will check you regularly for such side effects as high eye pressure. Because of the potential of side effects, it is not recommended you keep steroid eye drops around the house for whenever your eye(s) get red. When you are done with treatment, throw the eye drops away. |





 Your eye doctor will make sure that the cells in the anterior chamber of your eye are not associated with any problem of the Cornea, the transparent tissue in front of the iris. If the Cornea is involved, such as in the case of
Your eye doctor will make sure that the cells in the anterior chamber of your eye are not associated with any problem of the Cornea, the transparent tissue in front of the iris. If the Cornea is involved, such as in the case of
 Endophthalmitis is more commonly a complication of ocular surgery (such as Cataract Surgery) or penetrating injury. Of course, this infection would not be treated with steroids like most Iritis eye disease, but with the appropriate medication to combat infection.
Endophthalmitis is more commonly a complication of ocular surgery (such as Cataract Surgery) or penetrating injury. Of course, this infection would not be treated with steroids like most Iritis eye disease, but with the appropriate medication to combat infection.