Anterior Uveitis can be Chronic or Acute
Have you suffered from a deep, boring pressure type pain in one or both eyes? Have you had redness in one or both eyes? Have you been very sensitive to light? Has your vision been fluctuating along with these symptoms? You may be suffering from Anterior Uveitis.
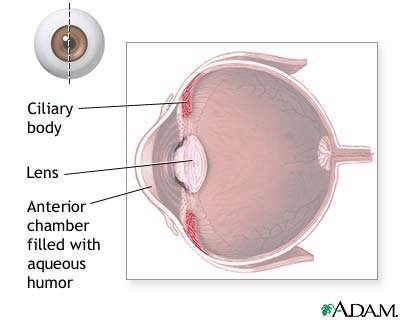
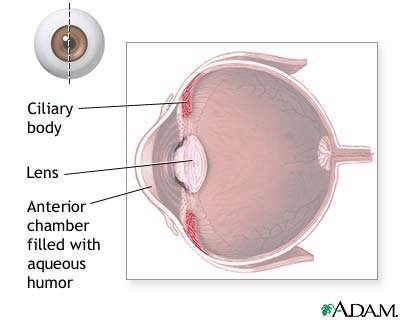
Anterior Uveitis is inflammation of uveal tissues inside the eye, mainly the iris (the colored part of the eye) and the ciliary body. The ciliary body is a pigmented, highly vascularized ring of tissue that encircles the lens. See image below.
The ciliary body has 3 functions in the eye:
1. Contains smooth muscle fibers called ciliary muscles that help to control the shape of the lens. This helps with focusing, or accommodation.
2. Toward the posterior surface of the lens there are ciliary processes which contain capillaries. The capillaries secrete the fluid (aqueous humor) into the anterior chamber of the eyeball.
3. Produce and maintain the lens zonules, which help in accommodation.
Anterior Uveitis may be associated with underlying systemic disease (e.g., an autoimmune condition) or it may occur as a direct result of ocular trauma. Occasionally, inflammatory reactions in adjacent tissues (like the cornea-keratitis) can induce a secondary Anterior Uveitis.Anterior Uveitis can be chronic or acute.
The chronic form has the following characteristics:
More often associated with a host of systemic disorders./LI>Most likely occurs due to an immunopathological mechanism that is not fully understood.
What are the signs and symptoms of Anterior Uveitis?
Symptoms of Anterior Uveitis include the following:
Deep, boring pressure type pain, location of pain feels like “in or behind” the eyeRedness: More often characterized by a circumlimbal flushPhotophobia (light is painful to the eye) Additional symptoms can include:
Variable visual acuityTearing resulting from increased neural stimulation of the lacrimal glandSigns of Anterior Uveitis include the following:
Hallmark signs are cells and flare in the anterior chamber (See diagram above.)The cells are usually white blood cells leaking from the ciliary body.The flare is protein leaking from the iris.Miosis: Pupil looks smaller than usualIntraocular pressure may be low (although it may be elevated)More chronic cases can show the following signs:
Fine keratic precipitates: Cells on endothelium that will appear to the eye doctor as discrete small dots less than 0.5 mm on the back surface of the corneaLarge “mutton-fat” keratic precipitates: Confluent, greasy and waxy looking deposits on the back of the corneaPosterior Synechiae: The iris sticks to the surface of the lensHypopyon: White blood cells accumulating on the bottom of the anterior chamber
How is Anterior Uveitis managed?
Anterior Uveitis is managed by reducing inflammation, preventing scarring and minimizing damage to the uveal blood vessels. Your eye doctor will begin treating this condition aggressively by prescribing steroid eye drops to be used every hour to two hours, depending on the severity of the presenting inflammation.
Like other situations where steroids are utilized, the steroid eye drops must be tapered slowly once the anterior chamber reaction improves. Steroids must be tapered in use instead of stopped all at once, even if the eye seems like it is white. The treatment course should at least last two weeks, but may be longer.
A tapering schedule may, for example, involve the dose being reduced to four times per day for a week, three times per day for another week, twice a day for another week, and finally once per day for another week before discontinuing.
For chronic cases, your eye doctor may prescribe a maintenance dose of once per day or once every other day in order to prevent recurrence.
Your eye doctor may also dilate your pupils to relieve the pain of iris muscle spasms and to break or prevent any adhesions between the iris and the lens surface.
How will you know if you should get further testing for any other health conditions?
If this is the first time that you have gotten this eye inflammation and it occurred only in one eye without any complications or any other complaints or symptoms, then no further work-up will be done.
If this eye inflammation has happened on more than one occasion, or it affects both eyes at the same time, then further testing should be done. More than likely a non-specific initial work-up will be recommended.
What type of tests will be done?
Complete Blood Count (CBC): This test is done to rule out any infection of the body or other more rare causes like leukemiaErythrocyte Sedimentation Rate (ESR): This test is done to detect active inflammation in the body. It does not specify the cause of the inflammation. When it is high, it suggests inflammation in the body. Antinuclear Antibody Test (ANA): This test is helpful when your doctor suspects an underlying autoimmune, collagen vascular disease. This test will not specify the cause of the disease, but it is most often used as one of the tests to diagnose Systemic Lupus Erythematosus. This test is also helpful in diagnosing Juvenile Rheumatoid Arthritis.Antinuclear Antibody Test (ANA): This test is helpful when your doctor suspects an underlying autoimmune, collagen vascular disease. This test will not specify the cause of the disease, but it is most often used as one of the tests to diagnose Systemic Lupus Erythematosus. This test is also helpful in diagnosing Juvenile Rheumatoid Arthritis.Rapid Plasma Reagin (RPR) or Venereal Disease Research Laboratory (VDRL): These tests are used to diagnose syphilis. If these are positive, the syphilis is active. Whenever a screening test (RPR, VDRL) is positive, a more specific test should be used to confirm the test.
More specific tests include:
Fluorescent Treponemal Antibody Absorbed (FTA-ABS) or Microhemagglutination Assay (MHA-TP): These tests are used to detect antibodies to the bacteria Treponema pallidum, which causes syphilis
Purified Protein Derivative (PPD): This PPD skin test is a method used to diagnose tuberculosis. Anergy panel testing is used as an additional test to confirm the diagnosis of tuberculosis since it can show whether your immune system is functioning properly or not, and so indicate whether the results of the other skin test are reliable. Anergy panel testing can also be included in the battery of tests used to diagnose Sarcoid. Sarcoid is a chronic inflammatory condition that can affect any part of the body, including manifesting itself in the eye with such inflammatory conditions as Anterior Uveitis. Sarcoid, like tuberculosis, can affect the lungs and so X-rays are an important additional test.X-rays: Can be used to diagnose the following conditions:
Ankylosing spondylitis: The sacro-iliac joints are located in the lower back. This condition shares many features with other arthritis conditions. It can cause inflammation in or injury to other joints away from the spine, as well as to other organs, such as the eyes, heart, lungs, and kidneys. X-rays would be done on the sacro-iliac joints.Chest X-rays can help diagnose:
SarcoidTuberculosisLyme titer: Checked in endemic areas. Human Leukocyte Antigen B27 (HLA-B27): This is not a definitive test, but is used as a piece of evidence in a constellation of signs, symptoms, and lab tests to support the diagnosis of certain autoimmune disorders such as:
Ankylosing spondylitis: Characterized by chronic inflammation of the spine and the sacro-iliac joints. See above. Inflammatory Bowel Disease (IBD): A group of disorders in which the intestines (small and large intestines or bowels) become inflamed.Psoriatic Arthritis: A painful, inflammatory disease of the joints that most commonly occurs in association with psoriasis of the skin.Behcet’s Disease: A rare, chronic inflammatory disorder.Although most cases of Anterior Uveitis resolve successfully and do not recur when managed properly, experiencing this inflammatory condition in the eye may not be necessarily benign. If you experience multiple episodes (three or more times) of Anterior Uveitis, suffer attacks in both eyes, or have associated inflammatory joint pain or intestinal problems, consider getting lab work and other pertinent tests to discover any underlying inflammatory disorder.
Return From Uveitis to Eye Diseases
Enjoy this page? Please pay it forward. Here's how...
Would you prefer to share this page with others by linking to it?
- Click on the HTML link code below.
- Copy and paste it, adding a note of your own, into your blog, a Web page, forums, a blog comment,
your Facebook account, or anywhere that someone would find this page valuable.