|
Dry Eye is Perhaps the Most Common Eye Condition
Do your eyes bother you? Do you experience a burning sensation in your eyes? Do you suffer from a sandy, gritty feeling in the eyes? Do your eyes water? You may have Dry Eyes (aka Keratoconjunctivitis Sicca). In order to view the content, you must install the Adobe Flash Player. Please click here to get started.
This is perhaps the most common condition that primary eye care providers encounter in daily practice and the single most common complaint among contact lens wearers. A little over a third of patients discontinue contact lens wear at least once, most frequently because of the symptoms of Dry Eyes. The tear film of the eye is one of the most important components to consider in evaluating for Dry Eyes. The tear film is an intricate entity that balances the structural integrity of its three layers; i.e., the mucin, aqueous and lipid layers. Each layer has a special role in keeping the eye moist and minimizing the evaporation of tears. Besides the tear film, the status of the cornea (the transparent tissue covering the iris), the conjunctiva (the clear tissue covering the white part of the eye), and the lid margins is integral to identifying and treating this eye condition. Are there factors that can be making your symptoms worse?
In adequately managing your Eyes, your eye doctor should assess the contributing risk factors that can make your symptoms worse. Medications can exacerbate Dry Eyes. Examples include: How are Dry Eyes diagnosed?
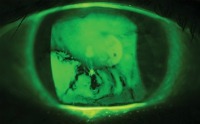
There is no single method used by eye doctors to determine if a patient is a candidate for dry eye therapy. Of course, your eye doctor will take into account your symptoms (such as burning, tearing, redness, etc.) and the clinical signs demonstrated by your eyes when deciding on a therapeutic regimen. There are four top favorite tests that most eye doctors may use to assess your Dry Eyes: The green dots in the image below are evidence of punctuate staining, a common finding in Dry Eyes. 
The dark areas show the drying areas in the tear film.
The green dots show staining of the conjunctiva indicating Dry Eyes. 
The thread is placed on the eye in the bottom under the lower lid to see how far the tears go down the thread. It needs to be in place for only 15 seconds and a reading greater than 10 mm is considered normal. What can you do for your Dry Eyes?
The answer to this question depends on the severity of your symptoms and clinical signs as well as the sum total of your risk factors. Knowledge is the key in addressing uncomfortable complaints. For example, once you find out that one of the medications you take is making your Eyes worse, then you are better prepared to deal with that side effect. Small modifications in your environment can potentially make a significant impact on tear film health. Knowing that extensive computer use, and the resulting decreased blink rate, places additional stress on your tear film will equip you with the tools to manage these conditions better. Although you cannot stop working on the computer, you can make sure that you have lubricating tears by your monitor to remind you to use them throughout the day. Consider moving your monitor below eye level since a computer screen positioned directly at or above eye level exposes more of the ocular surface between blinks. Redirection of upward-facing forced air vents at work and home should help reduce symptoms. Consider getting a room humidifier during dry winters and arid climates. You do not have to stop wearing contact lenses because you have Dry Eyes. As a matter of fact, soft contact lenses can be used as a bandage for some patients. If you have more significant cornea damage, your eye doctor may recommend a scleral contact lens. This large lens acts as a moisture chamber. The first line of defense in managing Dry Eyes is lubricating tears. If you use preserved artificial tears, use them up to four times per day. Using them more than four times per day can put you at risk to develop a toxicity reaction to the preservatives. Also, if you need to use the drops more than four times per day, your condition may be more severe than originally assessed. If artificial tears alone are not giving you the relief you wish, the second level of defense is proper nutrition and supplementation. Omega-3 fatty acid supplementation has become a staple treatment for Dry Eyes. Omega-3 fatty acids have been shown to decrease inflammation, stimulate tear production and thin meibomian gland secretions. Omega-3 fatty acids are available in eggs and fish like salmon. An excellent plant source of omega-3 fatty acids is flax seed. A recommended dose for supplementation is 1,000 mg to 2,000 mg per day. Because inflammation has been shown to be associated with Dry Eyes, do not surprised if your eye doctor recommends a course of steroid eye drops for about 1.5 to 2 months. The steroid drop will be used four times per day for a month before being tapered. If you experience significant relief from your symptoms with the steroid drops, then inflammation is a key component in your condition. Long-term use of steroids is not recommended because of potential side effects. Although infrequent, long-term steroid use can increase intraocular pressure and cause the formation of Cataracts. Restasis (cyclosporine 0.05%) is the only FDA-approved prescription medication for the treatment of Dry Eyes, which helps combat inflammation long-term without the steroid potential side effects. No treatment would be complete if an underlying lid condition goes untreated. The meibomian glands in the lids produce the tear film’s lipid layer. Direct heat with warm compresses is usually the first line of therapy to remove coagulated oils in the meibomian glands. Topical antibiotics may be prescribed as well. Further treatment, especially in light of lid disease includes using oral tetracyclines, not only for their antibacterial effects, but for their anti-inflammatory effects. Finally, once the tear film integrity is reestablished, the next goal is to retain the tears on the eyes for a longer duration. This can be done with punctual occlusion. Usually your lower punctum (the duct opening on the nasal corner of each lid margin where tears exit the eye) is occluded. Advanced treatment beyond the conventional treatment discussed above is not routine and is best discussed with your eye care provider. |