What is Blepharitis?
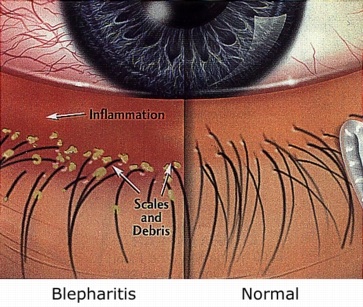
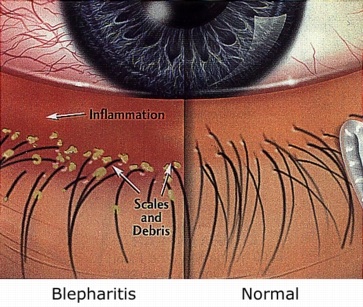
Blepharitis refers to a range of conditions characterized by dermatTitis or eczema of the eyelids that may be acute or chronic, with either inflammatory or infectious causes.
Because the eyelids play an important role in producing and distributing the tear film, blepharitis can affect vision by disrupting the surface of the cornea and the bulbar conjunctiva. Most forms are chronic although acute forms exist.
--
In order to view the content, you must install the Adobe Flash Player. Please click
here to get started.
Common classifications:
1. Staphylococcal
Usually caused by bacteria (staphylococcus aureus or staphylococcus epidermis)Produces a moderately acute inflammation of relatively short durationMore prevalent in warmer climates Most staphylococcal blepharitis occurs in younger females (mean age 42) who have no other skin abnormalitiesHordeolum and Chalazion may also occur Associated signs:
Lid swellingErythema of the lid margins (redness)Scaly debris and protein build-up (referred to collarettes) at the base of the lashesPossible skin ulcerationAqueous-deficient
dry eye
frequently results
2. Seborrheic Blepharitis
Associated with a skin disorder that includes the scalp, face, and eyebrows, all of which culture a normal growth of surface organismsThe base of the lashes are surrounded by greasy, foamy scales called scurfsThe foamy secretions can get in the eye and result in the complaint of burning of the eyesMore common in older adultsCan be associated with a secondary inflammation of the meibomian glands (oil glands found at the lid margins). This type of blepharitis is marked by sporadic episodes of clogged meibomian glands with lipid secretions of toothpaste consistency, producing an unstable tear film.
3. Mixed (Blepharitis)
Least commonAssociated with Seborrheic DermatitisChronic in natureAssociated with secondary infection of the cornea and conjunctivaInflammation is also involved
4. Meibomian Seborrheic Blepharitis
Can be identified by the presence of increased meibomian and seborrheic secretions without acute inflammationTears are sudsy and foamy, and as described above produce a burning sensation, especially in the morningLid glands are dilated, leading to copious meibomian secretions (oily discharge) and eye redness
5. Meibomian Keratoconjunctivitis
Also referred to as Primary Meibomianitis Blepharitis is the most severe lid margin inflammationTypically occurs in persons in their fiftiesMore common in colder climatesFrequently associated with acne rosacea, and is part of a generalized sebaceous gland dysfunction which clogs the meibomian openings with desquamated epithelial cellsBecause lipid secretions have a higher melting point than the ocular surface temperature, stagnation of free fatty acids within the gland and thickened openings of the gland result in a lipid-deficient tear film
6. Angular Blepharitis
Localized on the lid at the outer canthus (or corner of the eye on the ear side as opposed to the nose side) Categorized in two forms
Staphylococcal is typically dry and scalyMoraxella is caused by Morax-Axenfeld diplobacillus bacteria and is wet with a whitish, frothy discharge
What are the signs and symptoms?
Symptoms include itching, burning, foreign-body sensation, and sticky, crusted eyelids on waking. This chronic irritation leads to unconscious eye rubbing causing reddened eyelid margins or excessive blinking.
Flaky scales on lashes (resembling dandruff), loss of lashes, and ulcerated areas on lid margins are other signs of the condition. The degree of the inflammation will determine the severity of the symptoms.
Associated tear film disorders resulting in dry eyes can also occur. In more severe forms, secondary conjunctival and corneal inflammation and/or infection may occur.
How is it managed or treated?
Your eye doctor will perform a thorough external examination of the lids and other parts of the surrounding eye in order to determine the severity of the inflammation.
Daily cleaning of accumulated debris from the lid margins removes a potential breeding ground for microorganisms. Normal face washing, with attention to the surrounding eye area, is sufficient for most people.
However, if extra attention is needed to remove debris from the base of the lashes, there are a number of commercial lid cleansing pads available. Regular use of warm compresses is often helpful when you have clogged meibomian glands.
If you have a hordeolum or
chalazion,
you may find it helpful to use a hot compress twice per day. One way to ensure that the compress remains hot is to use a hardboiled egg wrapped around in a washcloth that allows enough heat to penetrate your lid.
Each type may require its own treatment:
1. Staphylococcal Blepharitis
Treatment includes an antibiotic ointment to control the infection, along with the lid hygiene described above. Antibiotic
eyedrops
can be used, but they do not work as well as ointments.Use artificial tears to alleviate symptoms of dry eyesIf corneal inflammation exists, topical steroids may be used with caution2. Seborrheic (Blepharitis)
Lid hygiene consisting of warm compresses and lid cleansing is indicated. The scalp and eyebrows should be washed with an antidandruff shampoo.For resistant cases, oral doxycycline (100 mg/day) for 3-4 weeks may be needed. It is not unusual for patients with this condition to require lower maintenance doses after tapering. This drug or its derivatives should not be given to children or pregnant women.3. Mixed (Blepharitis)
Appropriate antibiotic ointments are required. When the lid’s inflammation is better, resume lid hygiene practices. 4. Meibomian Seborrheic Blepharitis
Lid hygiene and shampoo regimen as described aboveMeibomian glands should be massaged or expressed to remove the plugs at the openingsAntibiotic or antibiotic/steroid ointment can be helpful5. Meibomian Keratoconjunctivitis
Responds to warm compresses and massage of the lid to express the meibomian contentsWhen infection is present, topical antibiotic or antibiotic/steroid ointments should be usedOral doxycycline may be beneficial, especially when acne rosacea is present. A lower maintenance dose may be needed for a longer period6. Angular (Blepharitis)
Both forms are treated with antibiotic ointment
Treatment of requires close, ongoing cooperation between patient and practitioner. Your eye doctor should discuss with you the rationale for treatment and the expected results. As you read above, the chronic forms of blepharitis require long term management of the condition as there is no cure for the chronic variations.
Return From Blepharitis to Eye Problems
Enjoy this page? Please pay it forward. Here's how...
Would you prefer to share this page with others by linking to it?
- Click on the HTML link code below.
- Copy and paste it, adding a note of your own, into your blog, a Web page, forums, a blog comment,
your Facebook account, or anywhere that someone would find this page valuable.